If you aspire to become a medical assistant you must have been wondering if you can start IVs to patients.
As healthcare needs continue to grow, medical assistants often find themselves performing an expanding range of responsibilities such as administration of intravenous (IV) therapy.
Intravenous therapy, commonly referred to as “IVs,” is a vital tool in medical practice used to administer fluids, medications, and nutrients directly into a patient’s bloodstream through a vein.
So, in this article, we’ll discuss IVs, the purpose of IVs in healthcare, common types, how IVs work and function, their components, and so on.
Moreover, we’ll also discuss if medical assistants can start IVs and if they can then when they can start.
Plus, we’ll also discuss their scope of practice by state, which states allow medical assistants to start IVs, and which states don’t.
So, let’s get started.

What are IVs?
IVs, short for intravenous, refer to the administration of fluids, medications, or nutrients directly into a vein through a thin tube or catheter.
“Intravenous” means “within the vein,” and this method delivers substances directly into the bloodstream, allowing for quick absorption and immediate effect, which is especially important in emergency or urgent medical situations.
Administering IVs requires skill and careful monitoring by trained healthcare professionals. Monitoring includes checking for complications like infections, phlebitis (inflammation of the vein), or extravasation (leakage of the IV fluid into surrounding tissue).
What is the Purpose of IVs in Healthcare?
IVs are one of the most efficient ways to deliver substances rapidly, allowing healthcare professionals to manage a wide range of medical conditions and support essential bodily functions in situations where other methods might not be effective.
From hydration to medication and nutrient delivery, IVs play a crucial role in both emergency care and routine treatments, offering precise control over dosage and absorption rates.
Here is the purpose of IVs in healthcare:
Fluid Replacement
The primary purpose of IVs is to deliver substances directly into the bloodstream for fast and effective results. One of the most common uses is hydration, where IVs are used to restore fluids in cases of dehydration due to illness, surgery, or physical exertion.
This rapid rehydration is particularly critical in emergency situations, where restoring fluid balance can stabilize blood pressure and support organ function.
Medication Administration
In addition to fluids, IVs are essential for administering medications, such as antibiotics, anesthetics, and pain relievers, that need to act quickly.
By bypassing the digestive system, these medications reach the bloodstream faster and with more predictable effects, making IVs ideal for acute and time-sensitive medical needs.
Nutritional Support
In cases where patients cannot consume food orally or absorb nutrients properly, IVs are used to deliver essential nutrients directly into the bloodstream, known as total parenteral nutrition (TPN).
This form of nutrition is critical for patients recovering from major surgery, trauma, or digestive disorders, ensuring they receive the calories, vitamins, and minerals they need for recovery.
Electrolyte Balance
IVs help regulate essential minerals like sodium, potassium, and calcium, which are vital for normal bodily functions, mainly muscle and nerve function.
Electrolytes like sodium, potassium, and calcium are often included in IV solutions to address deficiencies and stabilize physiological functions, especially after severe illness or injury.
Blood Transfusions
In emergencies or surgical settings, IVs allow for rapid blood transfusions, helping to restore blood volume and oxygen-carrying capacity in cases of severe blood loss, anemia, or surgery.
See: Can Medical Assistants Draw Blood?
Common Types of IVs
IVs are an invaluable tool in modern healthcare, providing an efficient and controlled method to deliver fluids, medications, nutrients, and even blood transfusions directly into the bloodstream.
There are various types of IVs used depending on the treatment requirements and the duration for which the IV therapy is needed.
Here are the common types of IVs:
Peripheral IV Lines
The most common type is the peripheral IV line, which is typically inserted into the veins in the hand or arm for short-term treatments, such as fluid replacement or medication delivery during a hospital stay.
Peripheral IVs are relatively easy to insert and remove, making them ideal for short-term use. However, for long-term therapies like chemotherapy or extended antibiotic treatment, central IV lines are preferred.
Central IV Lines
Central IV lines are inserted into larger veins in the body, such as the subclavian or jugular vein, and offer more stable and secure access for extended medication delivery.
These lines can remain in place for weeks or even months, reducing the need for repeated needle insertions. These lines are used for long-term therapy, such as chemotherapy or extended antibiotic treatments.
IV Push or Bolus
Another common type of IV is the “IV push” or bolus, where a specific dose of medication is injected all at once through the IV line. This method provides a rapid effect and is useful in situations where immediate response to medication is necessary, such as in emergency settings or intensive care.
IV Drip
Lastly, the “IV drip” is a slower, continuous method where fluids or medications are administered over a period, allowing gradual absorption. This method is frequently used for fluids, electrolytes, and certain medications that require steady administration over hours or days to achieve a therapeutic effect.
How IVs Work?
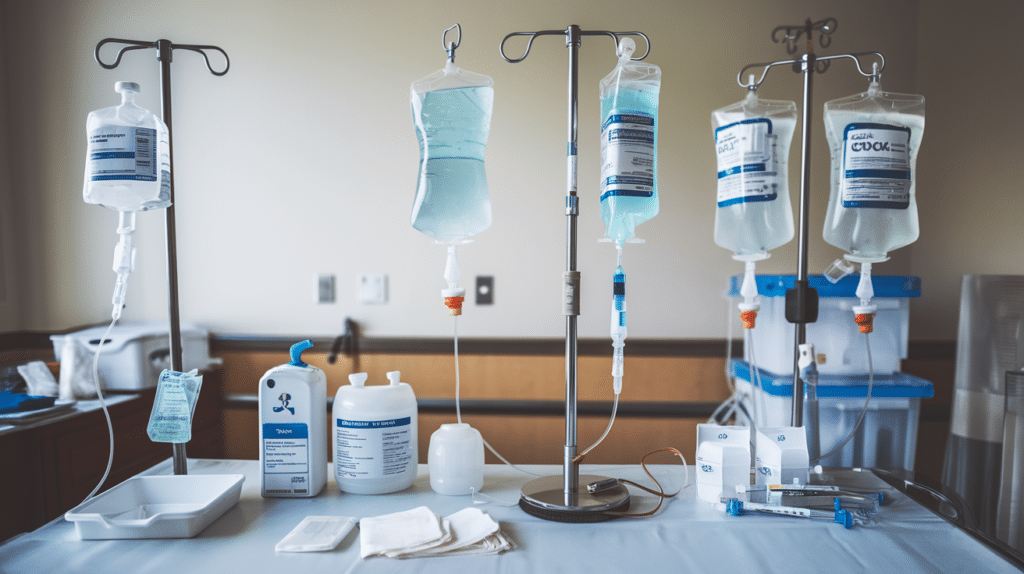
IVs, or intravenous therapy systems, are used to deliver fluids, medications, and nutrients directly into a patient’s bloodstream.
The basic idea behind an IV is simple, it allows healthcare providers to administer treatments quickly and efficiently by bypassing the digestive system, which can slow down the absorption of medications or fluids.
Here’s how IVs work, including the components of this commonly used medical device.
How IVs Function
IVs work by connecting a flexible, sterile tube to a needle or catheter inserted into a patient’s vein, typically in the arm or hand.
The catheter is connected to a bag containing the IV fluid or medication, which flows by gravity or is pumped into the bloodstream in controlled amounts.
The IV bag is connected to the catheter through the tubing, and it hangs above the patient to leverage gravity, allowing the liquid to flow downward into the bloodstream.
In some cases, an infusion pump is used to regulate the flow rate more precisely. The rate of delivery can be adjusted depending on the patient’s needs and the type of substance being infused.
The fluid flow is controlled by an adjustable roller clamp on the tubing, which allows nurses to increase or decrease the speed at which the solution enters the bloodstream.
This setup ensures a continuous, controlled infusion of the necessary substances directly into the bloodstream, allowing for immediate circulation and absorption by the body.
Here are the Components of an IV Setup
IV Bag
It contains the solution, which can range from simple saline to complex medication mixes.
IV Tubing
It connects the IV bag to the catheter, allowing for fluid delivery.
Roller Clamp
It controls the rate of flow into the patient’s bloodstream.
Catheter
A small, flexible tube is inserted into the vein to deliver fluids.
Needle (for insertion only)
Initially used to insert the catheter, then removed to minimize discomfort and allow the catheter to remain securely in place.
How to Administer IVs?
Administering IVs is a task that requires professional training and skill to ensure safety and effectiveness.
The first step in IV administration is preparing the equipment, which includes gathering the IV bag, tubing, and catheter, as well as antiseptic wipes, gloves, and tape.
After sanitizing hands and wearing gloves, the healthcare professional cleanses the area of the patient’s skin where the IV will be inserted, typically on the back of the hand or the forearm, using an antiseptic wipe to reduce the risk of infection.
Next, the catheter is inserted into the vein, which requires careful technique to avoid discomfort or vein damage. The healthcare provider gently inserts the needle at an angle, advancing the catheter into the vein once blood is seen in the catheter chamber, indicating successful vein entry.
The needle is then withdrawn, leaving only the soft catheter inside the vein, which is secured with adhesive tape to prevent movement.
After ensuring the catheter is securely in place, the IV tubing is connected to the catheter, allowing the fluid or medication to flow from the IV bag into the bloodstream.
The flow rate is adjusted to the prescribed rate, which can be controlled by an IV pump or manually adjusted depending on the setup and the patient’s needs.
Throughout the IV administration, the healthcare provider monitors the insertion site for any signs of complications, such as redness, swelling, or leakage, which could indicate infection or infiltration (fluid leaking into surrounding tissue).
Additionally, the patient’s overall response to the therapy is closely watched to ensure the treatment is progressing safely. When the therapy is complete, the healthcare provider removes the catheter, cleans the area, and applies a bandage to prevent infection at the insertion site.
Can Medical Assistants Start IVs?
Medical assistants play a crucial role in healthcare, supporting physicians and nurses with both administrative and clinical tasks.
As healthcare needs continue to grow, medical assistants often find themselves performing an expanding range of responsibilities. However, one procedure that often raises questions is the administration of intravenous (IV) therapy.
Whether medical assistants are allowed to start IVs depends on several factors, including state regulations, employer policies, and the level of training the medical assistant has received.
Understanding the limitations and requirements for starting IVs is important for anyone considering a career in medical assisting.
However, in most states, medical assistants are not permitted to start IVs due to legal and professional guidelines that govern their scope of practice.
IV therapy, which involves inserting a catheter into a patient’s vein to deliver fluids or medications, requires precise skill and thorough training to minimize risks such as infection, vein injury, or complications from fluid overload.
This task is generally considered beyond the basic training of a medical assistant and is reserved for licensed healthcare professionals, such as registered nurses (RNs), licensed practical nurses (LPNs), or paramedics, who have undergone specific training in IV therapy.
There are a few states where medical assistants may perform IV insertions, but this is typically allowed under direct supervision and in specific healthcare settings.
These permissions are often granted on a case-by-case basis and require the medical assistant to have additional certification in IV therapy.
However, even in states where it is permitted, healthcare facilities may have policies that limit IV insertion to licensed personnel.
The restrictions around starting IVs are in place to ensure patient safety and maintain a high standard of care, as IV administration requires knowledge of vein anatomy, fluid compatibility, and the ability to respond quickly to complications.
When Can Medical Assistants Start IVs?
While starting IVs is generally outside the scope of medical assistants, there are certain pathways that can make them eligible to perform this skill under limited circumstances.
To start, a medical assistant may seek additional certification in IV therapy. Some healthcare programs offer specialized IV training courses that teach safe and effective IV insertion techniques, as well as proper protocols for monitoring and responding to complications.
However, it’s important to remember that even with certification, state laws may still restrict a medical assistant’s ability to start IVs, and they must adhere to legal guidelines in their region.
Medical assistants who work in states that allow IV insertion for certified personnel may need to obtain permission from their employer.
See: Where Can Medical Assistants Work?
Many healthcare settings, such as hospitals or clinics, have strict protocols regarding who is authorized to start IVs, and medical assistants must have both state and employer approval to carry out the task.
In these cases, medical assistants often perform IVs only under the direct supervision of a licensed nurse or physician, ensuring that proper support is available if complications arise.
Some medical assistants who want to advance their skills and take on more responsibilities in patient care may consider enrolling in a nursing program.
Becoming a licensed nurse, such as an LPN or RN, provides the necessary credentials to perform IV therapy independently in most healthcare settings.
For those committed to a career in patient-centered care, nursing can open up a wider range of clinical opportunities, including administering IVs and other advanced procedures.
Scope of Practice by State
Medical assistants are integral members of the healthcare team, supporting physicians and nurses by handling a variety of clinical and administrative tasks.
However, the specific duties a medical assistant can perform vary significantly depending on state regulations. One area that often raises questions is whether medical assistants are permitted to start IVs.
Starting an intravenous line is a clinical procedure that requires skill and training, and the rules surrounding this task differ across states.
Understanding the scope of practice in each state is essential for medical assistants and employers to ensure compliance with legal guidelines and to uphold patient safety.
States That Allow Medical Assistants to Start IVs
Some states permit medical assistants to start IVs, typically requiring them to be under the direct supervision of licensed physicians and have received adequate training in IV techniques.
In the states where medical assistants may start IVs, they are often required to complete additional training or certification in IV therapy.
Furthermore, the procedure may need to be performed under the direct supervision of a licensed healthcare provider, such as a registered nurse or physician, to ensure patient safety.
These permissions are typically granted on a case-by-case basis, allowing flexibility for employers in certain clinical settings to assign IV tasks to medical assistants who have received adequate training.
States with more permissive regulations around IV administration for medical assistants may still require that these professionals be supervised and follow specific protocols to prevent complications and ensure high standards of care.
Even in states where IV insertion is permitted for medical assistants, individual healthcare facilities may enforce stricter rules than the state mandates, limiting this responsibility to licensed practitioners.
This is common in hospitals, clinics, and specialty practices, where policies prioritize patient safety and regulatory compliance.
As a result, medical assistants working in such states should confirm both state laws and employer policies before expecting to perform IV insertions.
These states include:
- Arizona
- Colorado
- Delaware
- Hawaii
- Idaho
- Indiana
- Iowa
- Kentucky
- Maine
- Mississippi
- New Mexico
- North Dakota
- Ohio
- Oklahoma
- Pennsylvania
- South Carolina
- Utah
- Vermont
- West Virginia
- Wyoming
States That Don’t Allow Medical Assistants to Start IVs
Other states strictly prohibit medical assistants from starting IVs due to the complexity and risk involved with this procedure, and they often reserve IV starts for registered nurses or physicians.
In states with strict regulations, Medical Assistants may not start IVs, even with specialized training. It’s essential for Medical Assistants and employers to understand their state’s laws to ensure compliance with medical regulations and maintain patient safety.
In these states, IV insertion is generally limited to licensed healthcare professionals, such as registered nurses, licensed practical nurses, or paramedics, who have received specialized training in IV therapy as part of their licensure process.
These states include:
- California
- Connecticut
- Florida
- New Jersey
- New York
- Alaska
- Mississippi (only in some settings)
- Texas
So, if you’re considering training as a medical assistant and are interested in starting IVs, it’s important to research state regulations and potentially pursue additional certifications that can expand your scope of practice where permissible.
Conclusion
We hope this article enlightens you on everything about IVs, whether medical assistants can start IVs, their scope of practice by the state, and much more.
Medical assistants are generally not permitted to start IVs, as this task is considered beyond their standard scope of practice, making it a responsibility typically reserved for licensed healthcare professionals.
For medical assistants interested in expanding their skills, additional IV therapy certification and employer approval may offer limited opportunities to perform IV starts under supervision, depending on state regulations and workplace policies.
Ultimately, if you want to become job-ready as a medical assistant faster, at an affordable price, without driving to a medical school then Preppy’s Self-Paced Medical Assistant Training Program could be the best option.
Read More:
- Types of Medical Assistants
- 12 Reasons to Become a Medical Assistant
- Top 10 Medical Assistant Benefits
- Registered Medical Assistant
Medical assistant





